TUESDAY, July 14, 2020 (HealthDay News) — About one-third of people prescribed drugs to prevent HIV stopped taking the medications when they were forced to stay home due to the coronavirus pandemic, a new survey finds. The reason, they said: They weren’t having sex.
Many discontinued the drugs without their doctor’s say-so, which has experts concerned.
“Reducing the number of new HIV transmissions and ensuring access to critical HIV prevention services must remain a public health priority during this challenging time,” said Bruce Packett, executive director of the American Academy of HIV Medicine.
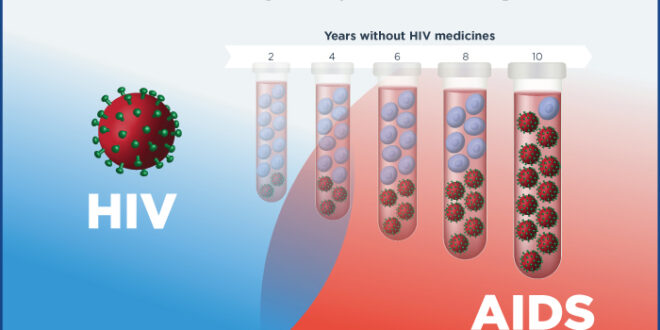
The online survey included more than 400 people at high risk of HIV infection who were using what’s called pre-exposure prophylaxis (PrEP) to protect them from the AIDS-causing virus.
Of the one-third who said they stopped the drugs due to shelter-in-place orders, 85% said they weren’t engaging in risky behaviors. That was the same overall rate among respondents.
Only 11 respondents said their ability to obtain PrEP was affected by a factor such as lost job/insurance, inability to get a refill from their doctor, or inability to complete laboratory monitoring or testing for HIV or another sexually transmitted infection.
More than half the respondents reported no sexual events and no sexual partners, while 89% said they’d reduced the number of sex partners. Ninety percent reported a decrease in the number of sex events, and 88% said they reduced the frequency of app use to meet partners.
The American Academy of HIV Medicine presented the findings last week at the virtual International AIDS Conference.
The academy also surveyed 188 PrEP providers to find out how social distancing policies in health care may continue to affect the drugs’ delivery. Nearly half said some of their patients had elected to stop their preventive medications during lockdown — even though nine in 10 providers didn’t recommend a change in medication routines.
Moreover, providers said they believe their patients are still engaging in risky behaviors, contrary to the patient survey.
“These data demonstrate the crucial role that technology-enabled care can play in helping facilitate the safe and timely delivery of critical public health services,” Packett added in an academy news release. “My hope is that clinics and HIV prevention providers can continue to adapt to changing circumstances by offering expanded use of telehealth services and other innovative tools to help meet the evolving needs of people at risk for HIV.”
Data and conclusions presented at meetings are usually considered preliminary until peer-reviewed for publication in a medical journal.
 Quelins – Relationship, Sex, Marriage and Health News around the world Quelins Blog is an online magazine about relationships, love, information about marriage, partnerships and issues patterning to all that.
Quelins – Relationship, Sex, Marriage and Health News around the world Quelins Blog is an online magazine about relationships, love, information about marriage, partnerships and issues patterning to all that.